
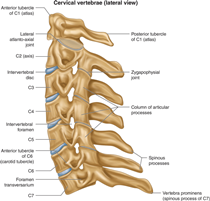
The cervical spine (neck) has seven different numbered spinal levels from C1 to C7. 
The craniocervical junction (CCJ) is the anatomic region located at the transition from the base of the skull to the upper cervical spine. In simple words, this is where the base of your brain becomes part of your spinal column.
Included in the craniocervical junction are the occipital bone, Atlas (C1), and Axis (C2), six synovial joints, and multiple ligamentous structures.
The Atlas (C1) and the Axis (C2), also referred to as upper cervical spine, are highly specialised and differ from the other 5 cervical vertebrae referred to as lower cervical spine (i.e. C3 to C7) in terms of anatomical structure and function.
The paired atlanto-occipital (C0–C1) and atlantoaxial (C1–C2) joints allow for significant multidirectional mobility at the craniocervical junction that is distinct from the subaxial spine (C3 to C7).
In fact, most of the cranial flexion, extension, and axial rotation is accomplished at the CCJ
⦿ Atlanto-occipital joint is responsible for almost 40% of flexion and extension movements.
⦿ Atlantoaxial joint is responsible for almost 60% of all cervical rotation
Craniocervical Instability (CCI) OR
Atlanto-axial Instability (AAI)

 Cervical instability occurs when the ligaments in between the base of your skull and the upper cervical spine are loose. These “lax ligaments” allow for excessive movement of the vertebrae at the atlanto-occipital joint and the atlanto-axial joint, that is, between the skull and the top two vertebrae (C1 and C2).
Cervical instability occurs when the ligaments in between the base of your skull and the upper cervical spine are loose. These “lax ligaments” allow for excessive movement of the vertebrae at the atlanto-occipital joint and the atlanto-axial joint, that is, between the skull and the top two vertebrae (C1 and C2).This can cause neuronal injury and compression of nearby structures including the spinal cord, brain stem, vertebral artery or vagus nerve, causing a constellation of symptoms. It is frequently co-morbid with atlanto-axial instability, Chiari malformation and tethered cord syndrome. It is more common in people with a connective tissue disease, notably Ehlers-Danlos Syndrome, osteogenesis imperfecta and rheumatoid arthritis. It can be brought on by a trauma, frequent whiplash; or other damage to the surrounding connective tissue.
CRANIOCERVICAL DISORDERS
Craniocervical junction disorders can cause headaches, pain and cervical instability. These types of disorders can happen at birth or develop after an injury.Some of the most common causes of Cervical Instability are –
Genetic Disorders- Ehlers Danlos Syndrome, or EDS, is the most common genetic disorder that causes CCI. People with EDS produce too much of a specific type of collagen, which causes the ligaments to be too stretchy. CCI is much more common in these patients, especially as they age. Klippel-Feil malformation, Down Syndrome and Platybasia are the other known congenital disorders that can cause CCI.
Trauma- Trauma to the cervical spine can cause cervical instability. For example, when a patient experiences whiplash during a car accident, the ligaments can be over extended and disrupted, leading to chronic cervical instability. CCI can also develop due to repetitive trauma over time.
Rheumatoid arthritis- The progressive deterioration of the joints and vertebrae due to Rheumatoid Arthritis can lead to cervical instability.
Symptoms
• Neck Pain• Headache
• Inability to hold up the head for an extended period of time
• Tightness or stiffness in neck muscles
• Instability/Dizziness
• Brain Fog
• Abnormal Eye Movements
• Double Vision
• Lack of co-ordination
• Voice changes
• Difficulty swallowing
• Respiratory problems or sleep apnea
• Weakness in limbs
• Ringing in the ears and hearing loss
• Nausea
Diagnosis
After the initial assessment by a doctor based on the patient’s symptoms, history, and other factors, advanced imaging studies are used to reliably confirm the diagnosis of cervical instability. Craniocervical junction disorders are usually diagnosed using imaging tests, which include:• Magnetic resonance imaging (MRI). Preferably Upright MRI with Flex Ext views.
• CT scan
• DMX to evaluate changes with movement
• Myelography with CT
• CT angiography
Important measurements used to diagnose CCI:
• Clivo-Axial Angle less than or equal to 135 degrees (indicates Brainstem Deformity)• Grabb-Oakes measurement greater than or equal to 9 mm (indicates Brainstem Compression)
• Harris measurement greater than or equal to 12mm
• Dens over chamberlain greater that 3 (indicates Basilar Invagination)
• Any spinal subluxation
TREATMENT OPTIONS:
1.) Physical therapy (traction, realignment and immobilization)2.) Surgery (Cervical Spine Fusion, Screw Rod Constructs, etc.)
3.) Prolotherapy (Regenerative Injections)
In craniocervical disorders, proper diagnosis is the key to direct patients towards the most appropriate and safe treatment options. The radiologist has a significant part to play in the appropriate management of patients who have suffered injury to this vital junction between the cranium and the spine.
Radiology 2nd Opinion Services
Our detailed radiology 2nd opinion reports thoroughly review your diagnosis, treatment options, and provide recommendations regarding your care, including answers to your personal questions.We offer:
1.) MRI 2nd Opinion
2.) CT Scan 2nd Opinion
3.) X-ray 2nd Opinion
4.) USG / Ultrasound / Sonography 2nd Opinion
5.) 2nd Opinion on Mammograms
6.) 2nd Opinion on PET Scans